Taken from: Exposing Spiritualistic Practices in Healing
by Edwin A. Noyes M.D., MPH
Chinese traditional medicine practices were little heard of in the West until the early 1970’s. I became involved in medical education in 1954 and not until the 1970’s did I hear of acupuncture or other traditional Chinese healing methods. The march toward scientific medicine in the first fifty years of the 20 century had been almost complete. The medical disciplines of eclectic medicine, homeopathy, osteopathy and naturopathy had either converted toward scientific medicine or had slowly faded and/or ceased to exist. Medical students were told about some past medical treatments, such as the use of heavy metals, emetics, blistering compounds, purgatives and bloodletting, but I heard no mention of Ayurvedic or traditional Chinese medicine, such as acupuncture or moxibustion.
Since the late 1970’s, there has been widespread acceptance of the oriental healing methods. Most of the older physicians rejected them, but a large number of younger doctors did not, and amazingly some of the alternative therapies have gone “main street.” For some practitioners, it has been mainly a financial interest; but for others, it has been a belief in these alternative methods. Now, we see in many medical training institutions and at the National Institutes of Health research being done on alternative treatment methods, acupuncture being one of the more common.
Segments of the Ayurvedic system have been used more widely than has Chinese traditional medicine. However, the Chinese methods are often used along with Ayurveda. Let us examine the roots of the traditional Chinese system of healing. You are probably very familiar with the symbol of two fish swimming in a circle with eight trigrams of all possible combinations of the two, which in Chinese is called pa kua and referred to in English as circle of harmony. Emperor Fu His, in 2900 B.C., is credited with its origination. It is a symbol representing all the conditions of interior—exterior, hot—cold, deficiencies—excesses, yin—yang. This Emperor’s works are the most ancient upon which traditional Chinese medicine is based. 1) Lyons, Albert S., Petrucelli, R. Joseph II; Medicine An Illustrated History, Harry N. Abrams, Inc. Publishers, NY, (1978), p. 125.
Another Emperor, Shen Nung, in 2800 B.C., compiled a text “pen-tsao” which was the first medical text for the use of herbs. It contained three hundred and sixty-five drugs, which he had tested on himself. 2) Ibid., p. 124.
The most celebrated ancient medical text in China is called the “Nei Ching.” It was written in 2600 B.C. by the Yellow Emperor, Hwang Ti. From this text is garnered information that gives us insight into the early approach to Chinese medicine and its orientation. 3) Ibid., p. 124.
January 1, 1912, Sun Yat Sen, a Western-trained physician, was inaugurated President of China following the revolution and over-throw in 1911 of the Imperial dynasty. Shortly following, he initiated improvements in hygiene practices in China such as having garbage cleared from the streets and installing running water in major urban centers

Picture of pa kua (circle of harmony)
A bureau to combat epidemics was established and Western style medical schools were developed by a few Western-trained Chinese physicians. The old practice of traditional Chinese medicine was discouraged and in 1929 outlawed. This caused a great furor from the traditional Chinese medicine doctors who banded together to fight the new restrictions. The masses of China were on the side of traditional medicine and the attempt to eradicate the old style practice failed primarily because of the belief of mostly uneducated Chinese masses in Taoism and the philosophy of “ch’i” with its “yin—yang” divisions. That attempt to modernize China failed.
The changes initiated by Sun Yat Sen were almost insignificant compared to the size and degenerate condition of the country. From 1916 until 1949 China suffered great political turmoil and instability, with minimal progress made in hygiene and health of the nation. Following Mao’s rise to power under Communism in 1949, public hygiene was made a priority. Eradicating the vectors of parasitic diseases, closure of open sewers, immunization programs, and clean water were measures taken to combat a deplorable health status, as documented by Paul Bailey in his book, A History of Chinese Medicine. He tells us of epidemics continuously of cholera, plague, black fever (500,000 afflicted in 1949), and 10,000,000 were infected by a parasite called bilhariza, 1,000,000 died each year from tuberculosis, epidemics of scarlet fever, and typhoid; untold millions were infected with malaria. The average life span was 35 years. This health status was a result of the mind-set of Taoism and the other Eastern religious concepts. The medical approach to illness was based on such beliefs which allowed these conditions to exist. Traditional Chinese medicine is based on Taoism (“The Way”). Three basic beliefs of Taoism, are:
-
-
The Creative Principle (or universal energy) is called ch’i and is composed of two parts–yin and yang (dualism);
-
Five basic elements are involved in transformation in creation:
metal, air, earth, fire, water. (these words represent “creative spirit power” from five planets
-
Man is the “microcosm” of the universe the “macrocosm.”
-
In contrast the Biblical account of creation tells us how God created:
For He spake and it was done and He commanded and it stood fast. (Ps. 33:9.}
Man was created by God forming the dust of the ground into man’s form; God breathed into it “the breath of life” and man became a living “soul.” Early on in the history of the world Satan’s counterfeit changed this story in such a way that left out the Creator, Jesus Christ the Son of God. This formed the myth of a great power, energy, voice, breath, that existed throughout space which was of two parts, good and evil that when it became properly balanced creation occurred. The Greeks called this cosmic spirit that they believed pervades and enlivens all things and produces change, “pneuma”, this equates with the Hindus’ “prana,” those of the South Seas “mana,” and the Chinese “ch’i.”
The Chinese explanation for origins is that with the proper balance of yin and yang (which are divisions of ch’i), transformation occurred which brought the cosmos, earth, and man into existence. Fundamental to traditional Chinese medicine is the astrological concept of the planets being closely associated with earth and man, with the sun and moon having the strongest influence. They had a belief in a “cosmological correspondence” between the houses of the Chinese zodiac and “chinglo channels” (now called meridians) that are said to be in man. Sheila McNamara, in her book, Traditional Chinese Medicine, makes the following statement:
To the Chinese, the human body is the cosmos in miniature. The universe is an organism and man is a microcosm of the universe…Yang is masculine: sun.…Yin is feminine: moon, 4) McNamara, Sheila; Traditional Chinese Medicine, Basic Books, [Perseus Books] New York, NY, (1996), p. 26. …
This belief gives expression in the saying “as above, so below.” This concept was prevalent throughout the ancient world but often expressed in different terms. A statement made by Gregor Reisch (c. 1467-1525) in Margarita Philosophica, published in 1503:
The pagans believed that the zodiac formed the body of the Grand Man of the Universe. This body, which they called the Macrocosm (The Great World), was divided into twelve major parts, one of which was under the control of the celestial powers reposing in each of the zodiacal constellations. Believing that the entire universal system was epitomized in man’s body, which they called the Microcosm (the Little World), they evolved that now familiar figure of “the cut—up man in the almanac” by allotting a sign of the zodiac to each of twelve major parts of the human body.
These beliefs led to “astrological medicine” which was dominant in Europe up until the 17th century. The physicians of that time used special “tables,” called “ephemerides or Alfonsine tables,” to make predictions based on astrological conjunctions, alignments and the angle between planets. These predictions were then used to perform various healing acts, such as drawing off blood from the body (venesection, cupping, causing great blisters to form), cauterization, surgery, and to choose herbs for medicines with special astral powers. Disease, they believed, came from an interruption of the free flow of “pneuma” or “prana,” as well as an imbalance of four body fluids called “humors.” Each humor was believed to be connected to a planet by correspondence.
To correct a supposed imbalance of “humors,” bloodletting (bleeding) was instigated and used by European and early American practitioners and is still done by some Muslims today.
…The practice of lancing, bloodletting and cupping, (hijama) to affect specific organs or to mitigate specific diseases based on a postulated relationship between the internal organs and points on the surface of the skin is still prevalent amongst the Muslims worldwide and nowadays video instructions for it are available, even on “YouTube.” It is plausible that the same principle is at the origin of acupuncture channels in China because the distribution of the regions of astrological influences and the related venesection points portrayed in medieval Islamic and European manuscripts significantly resembles the allocation of master, command influential, and other key points. 5) Kavoussi, Ben MS, MSOM, Lac, Science-Based Medicine, Astrology with Needles, pp.5,6; http://www.sciencebasedmedicine.org/?p=583 …
The Chinese followed a similar concept and saw disease as being a result of disharmony in the balance of yin and yang. This imbalance can occur for many reasons, such as lifestyle. It is believed that some physical disorders are caused by “winds.” Foods are considered yin or yang and the balance of such will influence so as to maintain health, or imbalance to allow illness. The beliefs of what causes imbalance in the yin and yang of the body are complex. I will not go into the causes of imbalance, but rather will direct our attention to the practices that are said to be capable of restoring balance.
In Ayurveda, prana, universal energy is said to be centered in whirling vortexes of energy referred to as chakras. The flow of energy through the body is said to be facilitated by meditation, yoga exercises, diet, herbs, essential oils aromatherapy, and cleansing therapies. In traditional Chinese medicine (TCM) the energy is described as flowing through the body in “meridians” which are (imaginary) channels perpendicular to the body. Many smaller channels branch from the meridians and distribute the energy throughout the body. Here too, meditation, exercises, food—drink, moxibustion, acupressure, acupuncture, and other sympathetic remedies are used to facilitate the flow and balance of ch’i.
All creation depended upon correspondence, association, and sympathy between the various phases outlined above and yin—yang balance of ch’i. All disease of animal and man is considered to be an imbalance of yin—yang. Correcting the imbalance is believed to restore health, therefore methods to balance ch’i and treat disease were developed over millennia of time.
Diseases are classified according to four different states of disharmony and make up eight syndromes, which include all varieties of disease. These previously mentioned conditions are: imbalance of yin/yang; interior/exterior; hot/cold; and deficiencies/excesses.
The customary way to diagnose an imbalance of energy in traditional Chinese medicine was to observe the tongue and feel the pulse. The tongue was felt to demonstrate changes in energy (ch’i) distribution throughout the body. Taking the pulse was done not to check the rate and rhythm of the heart, but to find where an imbalance of ch’i existed. One ancient author of Chinese traditional medicine wrote ten large volumes on pulse diagnosis. From the pulse and observation of the tongue, those physicians determined the imbalance of ch’i (qi), where it existed, and then prescribed to balance it.
DISEASE TREATMENT METHODS
In this chapter is presented those methods of treatment most commonly known and accepted by Western society. These include the use of herbs, martial arts and acupuncture. The Chinese practice disease prevention, with special emphasis on exercise and diet. Disease prevention is directed toward maintaining a balance of body energies.
In traditional Chinese medicine, herbs and foods are considered to have a “signature” and “like cures like.” For instance, walnuts resemble the brain therefore walnuts are especially nourishing to the brain. For a child to eat the pig’s tail, is to assure a straight, strong spine as he or she grows (in China pigs have straight tails). If an herb looks like an organ of the body, then it is considered to have special healing powers for that part of the body. 6) McNamara, op. cit., p.117
Ginseng root can resemble the body and its limbs and is therefore considered good for all bodily ailments. The horn of an animal represents a phallic symbol and so is used as an aphrodisiac. Consumption of animal parts, such as a tiger’s heart, will give courage. This type of belief has resulted in a large number of herbs being used because of their appearance rather than from their biochemical properties. Many animal parts are likewise used in this way. I visited a very large Chinese pharmacy in Vancouver, British Columbia, Canada, and was amazed to see dried parts of animals, fish and many other products I could not identify. The store had a thousand or more different substances, some in bottles and some in open boxes.
The idea of “like cures like” is an association–sympathy concept and not at all due to the chemical action of our systems. The Chinese found many herbs and substances that really do have significant biochemical action which are used world-wide. Herbal books will often label herbs as either hot–cold and/or yin–yang. The herbs may then be chosen for medicinal use accordingly so as to influence a sick person’s balance of yin-yang and or hot and cold.
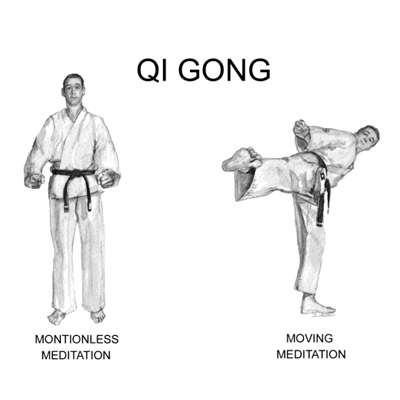
MARTIAL ARTS—QI GONG
Qi gong is the forerunner of traditional Chinese medicine, since qi/ch’i, the subtle breath, or life energy, is at the heart of everything. 7) Ibid., p. 130.
Qi gong or (Ch′i Kung) means manipulation of vital energy (psychic energy), and is also the precursor of martial arts that have been practiced in China for hundreds of years. Qi is comprised of yin and yang, each contributing to health when in proper balance. Gong refers to achieving the ultimate balance of the two parts. Qi gong is a variety of physical exercises and actions practiced to facilitate the harmony of yin and yang. If one is able to superbly balance these parts of qi, he will be able to accomplish extraordinary feats with his powers and will be a master of qi gong.
Qi gong is a system of body/mind discipline of traditional Chinese medicine and is the foundation of martial arts, which are practiced under various names, such as ninjutsu, tai chi chuan, ikido, tae kwon do, judo, kenpo, karate, etc.
Fundamentally, qi gong is a method of meditation exercise aimed at the cultivation of physical and spiritual perfection. 8) Ibid., pp. 127–128.
Meditational forms involve stillness, standing, sitting, or lying motionless. More physically active forms will involve breathing exercises in order to inhale the “vital essence of life.” Physical activity is frequently a slow, smooth, and rounded movement. Concentrating on breath and emptying the mind are very important. These activities are “always with a spiritual element”. 9) Ibid., p. 128.
The exercises can be performed alone, or by a qi gong Master for another person, which involves exercising around the other person’s body, without making any physical contact. This is supposed to activate the qi within another’s body so that the person can be brought into the qi gong state.
Balancing the qi is the objective, for too little qi is equivalent to illness. When people do their own exercises, or when masters do the exercises for them, qi, it is said, can be directed towards different areas within the body.
Martial Arts — Tai Chi
One of its main precepts concerns finding the center of the body, to attain perfect balance as a prerequisite to health. Students will be taught to visualize the soles of their feet reaching hundreds of yards deep down into the earth, or a rod passing down their spine via entering of their head and penetrating deep into the ground. Once they achieve perfect balance, no one will be able to knock them off-balance. It proves that the qi is perfectly centered, neither too weak in one part of the body nor too strong in another. 10) Ibid., p. 128.
I once presented this information to an assembly and a gentleman came to me afterward. He spoke of taking karate, one of the disciplines of qi gong, and how he and two other students tried to push their instructor off-balance and were unable to do so. The question to ask is, what power held him to the ground?
A delegation of Chinese physicians traveled to the United States to present to American doctors this particular aspect of traditional Chinese medicine. They desired to convince the American doctors of the scientific basis of this therapy for which they made great claims. They described studies showing that the power associated with this life force showed up as making changes in electrical brain wave potential; in the molecular rotation of liquid crystal molecules; and in cancer cells, bacteria, and viruses. The following was reported in The Medical Tribune:
After the Chinese Qi Gong scientists described their research, Dr. Li Xiao Ming, a Qi Gong master at the Qi Gong Research Institute at the Beijing College of Traditional Chinese Medicine, demonstrated his art on Dr. Alfonso Di Mino. As Dr. Li did his exercise around Dr. Di Mino, Dr. Di Mino shouted for Dr. Li to lower his hands as he said that he felt as if he “were ready to fly.” Later he said that it felt as if he had an “electric magnetic power inside his body” “My mind was not aware of my body.”
Dr. Di Mino, a biophysicist, described this “life force” as “the medicine of the future.” 11) Medical Tribune, Feb. 5, (1986) by Elizabeth Mechcatie (medical newspaper)
Robert Leeds, the vice chairman of the Sino-U.S. Qi Gong Center, then told the audience that Dr. Li was able to:
…manipulate energies we allegedly are not sensitive to or do not understand.” He added that for four thousand years, “the Chinese have been able to map out this energy field and manipulate it to such an extent that it can heal. “ 12) Ibid.
All across China in the early morning, people can be seen outside practicing various exercises of qi gong. All qi gong methods are supposed to produce equal flow of energy through the body and thereby promote health. Remember, there is a spiritual aspect connected to qi gong exercises. 13) McNamara, op. cit., p. 128.
Tai ch’i is one of the popular styles of qi gong. It is felt to be totally free of any spiritual association by most people practicing it. Sheila McNamara in her book, Traditional Chinese Medicine, says of the different qi gong exercises:
…but they all spring from the same ancient root, and all are based on the meridians which interconnect the internal organs and viscera with the exterior of the body, through which the qi flows. 14) Ibid., p. 128.
In U.S. News and World Report, Feb. 22, 1999, there was an article by Bay Fang, entitled An Opiate of the Masses? This article referred to an advanced type of qi gong exercise. Grand Master Li Hongzhi leads sixty million Chinese in the practice of Falun Gong “Rotating the Law Wheel.” Tape recordings of the voice of the Master were played as thousands gather to do exercises. With eyes closed the people raised their arms together and in perfect unison their hands swept slowly in a circle and came to rest in a prayer position.
Adherents in China say the Falun Gong Master can cure cancer, heal the blind, and make white hair turn black. …Throughout history, Qi Gong masters have captivated the public with their miracle cures, soothsaying and other tricks ranging from levitating objects to communicating with aliens and changing the odor of cigarettes. 15) U.S. News and World Report, Opiate of the Masses, by Bay Fang, Feb. 22, (1999), p. 45.
Martial Arts
We have seen how energy manipulation has progressed from the use of hands and needles, to exercises, and finally to energy manipulation without touching, just by using the mind to bring about “miraculous” changes. This type of progression, in whatever art being practiced, proves that the method used is not the real power, but is, instead, the mental connection with hidden powers of the occult.
ACUPUNCTURE AND CHINESE PHYSIOLOGY
Chinese physiology has astrology as its foundation. All qi gong exercises are based on the Chinese concept of physiology which teaches that there are fourteen meridians. Qi is believed to circulate through these meridians–the invisible lines of energy channels which are said to travel through the system–six on each side, one in the middle of the front, and one in the middle of the back. They run perpendicular on the body and have multiple small channels which connect to various organs of the body. Acupuncture is performed by needling these meridians at specific points in order to balance the distribution of energy (qi) to organs. Those who are proficient in qi gong can bring about this same balance simply by mind power and without needles.
The Chinese describe the distribution of ch’i (life energy) in a manner different from the Ayurvedic system. It is believed that the energy comes close to the skin in various places and can be influenced in those areas to alter its flow.
Stephen Basser M.D. did a very extensive review of studies evaluating acupuncture. His report “Acupuncture: A History,” appeared in the Spring/Summer issue of The Scientific Review of Alternative Medicine, 1999. He learned from his research that in the early 1970’s, manuscripts dating from 168 B.C., describing medicine as it existed in the third and second centuries B.C., were discovered in China at the Ma-wang-tui graves. From these manuscripts, descriptions of all procedures used in Chinese medicine during that period of time were obtained. Acupuncture was not mentioned. It first showed up in the Shi-chi text in 90 B.C.; however, there are descriptions of sharp stones being used to drain blood from veins prior this date. 16) Basser, Stephen M.D.; Acupuncture: A History, Acupuncture Watch; http://www.acuwatch.org/hx/basser.shtm Feb. 22, (2005).
The Ma-wang-tui texts describe eleven ‘mo’, or vessels, that were believed to contain in addition to blood a life force known as ch’i or pneuma. 17) Epler, Jr DC., Bloodletting in early Chinese medicine and its relation to the origin of acupuncture. Basser, op.cit. p. 1
It was not appreciated at that time that blood circulates in a closed system. The most important text of the end of the first century B.C was the Huang-ti nei-ching. It describes twelve vessels (mo) instead of eleven, and gives different courses for the vessels from those given in the earlier descriptions. The vessels are called “conduits” (ching) or “conduit vessels” (ching-mo); by this time it was understood that blood flows through a system where the vessels interconnect. The text also tells of a large number of holes located over the body of these vessels. At the time of this text, there was no distinction made between vessels on the basis of content, and no explanation as to how the blood and ch’i circulated in the vessels. The texts reveal that the belief later developed that ch’i flowed through a separate system of vessels (today called meridians) which did not contain blood. 18) Bassar, op. cit., p. 2.
Early in the history of Chinese medicine disease was attributed to imbalances of ch’i, and was caused by demons (hsieh-kuei); and that demons were carried by winds, and that winds dwelt in caves or tunnels. The demons (evil spirits) were believed to lodge within the vessels carrying ch’i and disturbing the flow. To dislodge the demon which was clogging the flow of ch’i, needles were inserted in the holes (tunnels) over the vessels allowing escape of ch’i and relieving the congestion. 19) Epler, Jr DC. Bloodletting in early Chinese medicine and its relation to the origin of acupuncture. Bull Hist Med. 1980l54L357-367; Reported in Basser, Ibid., p. 2
The vessels, and not the openings, were the central feature of “ancient” acupuncture, whereas in modern practice the points appear to be of prime importance. The vessels have, over time, lost their association with the vascular system and in the West are now viewed primarily as functional pathways lining the openings. The term “meridian” rather than “vessels” merely serves to aid in clouding the issue. 20) Unschuld PU. Medicine in China: a History of Ideas, Berkeley, CA: University of California Press; (1985), Reported in Acupuncture Watch; Basser, op. cit., p. 2.
Pulse diagnosis was developed during the time that ch’i was believed to flow through blood. It was believed that the location of blockage of ch’i could be determined by feeling the pulse.
Acupuncture Points
Over time the connection between needling and ch’i, which formed the basis of acupuncture, was described in the context of an emerging cosmological view of the world, not evident in the earlier descriptions of medical bleeding. Organic medicine was subsumed under this emerging system of cosmological correspondences. 21) Unschuld PU. Nan-ching: The Classic of Difficult Issues. Berkeley, CA: University of California Press, (1986), p. 5; Reported in Basser, op. cit., p. 2.
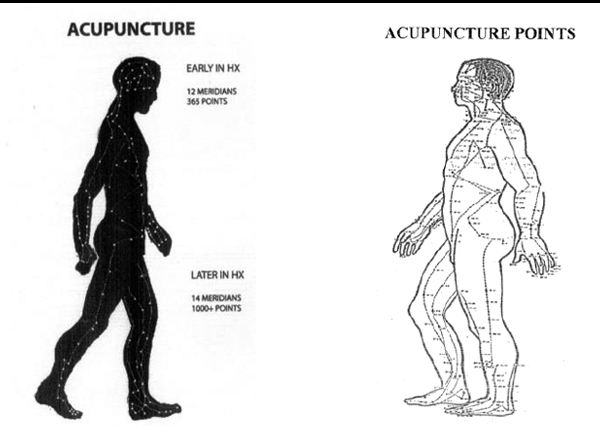
Early in the history of acupuncture, there were twelve meridians and 365 points, one point for each day of the year. This has changed and now many more points and fourteen meridians are said to exist. The body is supposed to have twelve organs. The Chinese day is considered to be twelve hours which covers the 24 hours we have in a day. One hour of Chinese physiology time equals two hours of our time. The ch’i is claimed to flow around through the twelve organs, on schedule, where one organ will have the dominance of ch’i for one Chinese hour (two hours), then another organ, so covering all organs in twelve divisions of the day. This is analogous to the zodiac and the planets, and reflects the belief that man is a small cosmos.
Acupuncture at specific points is believed to cause a change of the energy (ch’i) flow running through that specific point to bring a desired balance of the yin and yang. This method is used for all types of illnesses, even for overcoming habits such as smoking. Some people claim to have experienced great relief from pain. Others have stopped smoking. What are the believed causes of the presumed imbalance of energy which results in disease? Lifestyle, different foods, and many other things are believed to influence the balance of energy. Winds are also believed to be a source of over 100 different diseases.
Treatment entails balancing the energy (ch’i), or using Like Cures Like therapy. Prevention involves meditation, and/or meditation in exercise, and balancing the yin—yang of food. It is also important to have balance in the home, such as the proper placement of furniture.
As mentioned previously, energy balancing techniques of Chinese traditional medicine are as follows: meditation, meditation in exercise, breathing exercises, qi gong, tai ch’i and martial arts of all types, diet, drugs, minerals, herbs, moxibustion, acupressure, and acupuncture. Acupuncture is by far the most popular healing methods of traditional Chinese methods in the West. Today the proponents of acupuncture commonly use the term “energy” in referring to
ch’i, however this is misleading as:
The core concept of ch’i bears no resemblance to the western concept of energy (regardless of whether the latter is borrowed from the physical sciences or from colloquial use.) 22) Unschuld PU. Nan-ching op. cit., p. 5; Reported in Basser, op. cit., p. 2.
This is true in Ayurveda (prana) as well as traditional Chinese medicine. The Christian believes in a God of Creation who, by the power of His spoken word created the heavens and the earth. The universe and man are sustained by His power, as is healing. And salvation of man is obtained through faith in the belief in the life, shed blood and death, and resurrection of Jesus Christ.
The pagan denies the living God (Trinity), yet he recognizes there is a power that created and sustains the universe. We learned in chapter 4 of his explanation for creation, of the vital force believed to sustain us, and of the balancing of the supposed force’s two (yin—yang) divisions to heal. This power was considered a spiritual force; therefore a system was devised whereby man believed he could manipulate and influence this power to sustain well-being, to heal, as well as to obtain eternal life.
The creative power of God is not measurable or demonstrable by mechanical measuring instruments, and is not under the control of man. This power, which paganism separated from God, had many names, such as vital force, prana, ch´i, qi, and more recently, universal energy. The term “energy medicine” is commonly used to refer to the various techniques used in holistic health therapies. Scientists who are believers in these theories desire to show that this power (ch´i) is truly in the field of modern science and attempt to measure and demonstrate such. It is most likely that the common use of the term “energy” in reference to the “vital force” power has come from this desire. To the established believer in Hinduism or Taoism, the term “energy” may be an insult to his beliefs. The words prana, ch´i or qi, mana, etc. are not true synonyms of the word “energy.”
DOES ACUPUNCTURE WORK?
Acupuncture seems to do something for some people but nothing for others. Could it be a placebo effect? Why have we not had studies that really determine if it works by the placebo effect or not? Part of the confusion and lack of solid “yes” or “no” answers rises out of the difficulty of doing quality scientific studies on this procedure. It is difficult to do a “mock” acupressure or acupuncture procedure. However, hundreds of studies have been done to test the effectiveness of the procedure over the past 35 years.
In 1981, the Academy of Sciences of the German Democratic Republic produced a statement regarding the effectiveness of acupuncture. Their summary, written by Rudolph Baumann, and published in Zeitschrift fur Experimentelle Chirurgie 14:66-67, 1981, concluded the following:
-
- Points of acupuncture are unknown to science and are not demonstrable, and different schools of acupuncture have charts that do not match for specific points.
- All procedures attempting to prove their presence have failed.
- Equal effects are obtainable in acupuncture when no attention is paid to specific points on the body.
- There is no benefit to be expected to organic disease.
- Infectious diseases have no response to acupuncture.
- Acupuncture does not give better results than hypnosis, suggestion, or autosuggestion.
- There was not enough evidence of effect to recommend research or to teach the subject to medical students or physicians.
Dr. Basser reported in 1999, that:
Carefully designed and conducted scientific studies have so far failed to demonstrate that the Chinese acupuncture is associated with more effective pain relief than either placebo or counterirritant stimulation such as TENS (transcutaneous electrical nerve stimulation). 23) Ibid., p. 6.
TENS has been used for many years for mild to moderate chronic musculoskeletal pain. Basser has concluded that from a scientific viewpoint it can now be said with confidence:
-
- The concept of ch’i has no basis in human physiology.
- The vessels, or meridians, along which the needling points are supposedly located, have not been shown to exist and do not relate to our current knowledge of human anatomy.
- Specific acupuncture points have not been shown to exist—as noted earlier, different acupuncture charts give different numbers and locations of points. 24) Basser, op. cit., p. 8
For the past thirty years science has not been able to explain the physiologic actions from acupuncture or to detect any true lasting value from the use of acupuncture. Many proponents of this technique will rise up in alarm by this statement, but this is what I have found.
In November 1997, The National Institute of Drug Abuse held a Consensus Conference on acupuncture. The meeting was arranged by a Dr. Trachetenber, who is reported to be a strong advocate of acupuncture. Wallace Sampson, M.D., FACP, presents a critique of the conference, in Acupuncture Watch. 25) Sampson, Wallace I. M.D.; Acupuncture Watch, Critique of the NIH Consensus Conference on Acupuncture, March 2005, p. 2; http://www.acuwatch.org/general/nihcritique.shtml He mentions that the first question that arose was, why investigators who had previously made studies on acupuncture, which showed no measurable effect from acupuncture, were not a part of the presenting scientists. There seemed to be present only proponents of acupuncture. Prior analyses of research of acupuncture (1986, 1988, 1990) had revealed that the best quality of research showed negative effects, and the low quality studies were mostly positive.
Dr. Sampson makes the following comment:
The lack of critical, scientific thinking was apparent in the panel’s report, which was sixteen pages long. It obviously was composed before the conference and changed somewhat after the presentations. Despite the uneven literature and the lack of firm evidence to support the conclusions, the consensus statement panel recommended acupuncture for musculoskeletal pain, some headaches, and nausea. It recommended use for nausea due to Chemotherapy, based on only three papers. 26) Ibid., p. 2.
Dr. Sampson continues:
That the consensus Conference was engaged in pseudoscientific reasoning is further illustrated by the rejection of the most obvious and probable reason for perceived effects. Those are natural history of the disease, regression to the mean, suggestion, counter-irritation, distraction, expectation, consensus, the Stockholm effect (identifying with and aiding the desires of a dominant figure), fatigue, habituation, ritual, reinforcement, and other well-known psychological mechanisms. With such an array of obvious alternative interpretations and such fertile areas for productive research, strong bias would be needed to agree to the conference conclusions.
Why would physicians make a consensus statement labeling acupuncture as being scientific if there is really no hard data confirming it? There could be several reasons, among which is the desire to place it in an acceptable light with patients and the scientific community. Those physicians who believe in Eastern mysticism and practice its techniques, do not enjoy being considered as on the fringe of scientific medicine; so when an organization such as the National Institute of Health puts out a consensus opinion that acupuncture is science-based this elevates its status. Also, if there is a consensus from an influential medical body that a particular procedure is science-based, it is easier to persuade insurance companies to pay for its use. Acupuncture is cheap to perform, the risks are low, it is popular, and the financial returns are very good. Never underestimate the financial interest.
Reports of studies testing acupuncture, some with positive results as to benefit over and above more conventional methods continue to appear. Most of these studies are dealing with discomforts and disorders that have strong subjective type complaints. These include headaches, a variety of aches and pains, etc. To do true double blind studies with acupuncture is almost impossible. There have been some sham acupuncture studies where the patients cannot detect if the needle is inserted or not and other studies that place needles anywhere but on the acupuncture points. The results of the sham and wrongly placed needles compared to the correct acupuncture procedures are almost the same. Do they work? Yes, many times, as do the fake procedures. I have never seen a study done using acupuncture for pneumonia, diabetes, coronary heart disease, meningitis, or other serious disease. We have had studies going on for forty years and still the results are questionable. If it is so good should it not be easy to show a difference, a large difference, using acupuncture versus not using it?
A positive report on a review of fifteen studies made by Duke University Medical Center in North Carolina, of the use of acupuncture for post surgical pain and which was reported on the Internet by Reuters Health Service on October 17, 2007. Acupuncture was done before and after surgery. There was less pain on those receiving the acupuncture than the controls but not freedom from pain. There was less nausea, dizziness, and also of urinary retention. Urinary retention often occurs with abdominal surgery due to reflex from pain.
Remember, surgery has been done on people using acupuncture as the anesthetic, so too was surgery done without pain in years past in India by use of hypnotism. In the report by Reuters Health a comment is made that doctors at the National Institutes of Health do not understand how acupuncture works. Many proponents of acupuncture will claim that the case is settled and may give you answers as to how they believe it works. In the following paragraphs I will share with you information as to that which is known about possible physiologic actions of acupuncture. This information comes from the New England Journal of Medicine, July 17, 2010/363:454-61. I obtained a report of a study done in 2008 and reported in Science Daily, January 21, 2009. I will share with you the report:
Headache sufferers can benefit from acupuncture, even though how and where acupuncture needles are inserted may not be important. Two separate
systematic reviews by Cochrane Researchers show that acupuncture is an effective treatment for prevention of headaches and migraines. But the results also suggest that faked procedures, in which needles are incorrectly inserted, can be just as effective.In each study, the researchers tried to establish whether acupuncture could reduce the occurrence of headaches. One study focused on mild to moderate but frequent ‘tension-type’ headaches, whilst the other focused on more severe but less frequent headaches usually termed migraines. Together the two studies included 33 trials, involving a total of 6,736 patients.
Overall, following a course of at least eight weeks, patients treated with acupuncture suffered fewer headaches compared to those who were given only pain killers, In the migraine study, acupuncture was superior to proven prophylactic drug treatments, but faked treatments were no less effective. In the tension headache study, true acupuncture was actually slightly more effective that faked treatments. 27) Linde K, Allais G, Brinkhaus B, Manheimer E, Vickers A, White AR. Acupuncture for tension-type headache. Cochrane Database of Systematic Reviews, Issue 1. Art. No.:CD007587 DOI: 10.1002/14651858.CDOO7587 Linde K, Allais G, Brinkhaus B, Manheimer E, Vickers A, White AR. Acupuncture for tension-type headache. Cochrane Database of Systematic Reviews, Issure 1. Ar. No.:CD001218 DOI. …
Why are we so hung up on using something that is so difficult to prove as to whether it has true benefit? If this procedure is what I understand it to be, then if I choose to use it I have subjected myself to the influence of Satan’s counterfeit healing system, with little chance of true lasting benefit above that of a fake procedure. We know that it has been used as an anesthetic wherein people undergo surgery and are wide awake and even can eat during a surgical procedure. Is there power in acupuncture? Yes, but whose power? The results of applying acupuncture may well be as dependent upon the connection of the therapists to the powers of the occult as the Theosophy Society states that radiesthesia is in radionics. (see Divination chapter). Studies on acupuncture never consider this factor.
In 1893 and 1958, the British Medical Society and the American Medical Society, respectively, made a consensus statement on hypnosis as being based in science even though there were no explanations as to how it worked. That it worked no one disputed, yet the Christian may recognize the source of its power as of the occult. (see chapter on hypnosis). I have observed reports on acupuncture for more than forty years, waiting for the definitive evidence that this technique works in the hands of anyone (not just sensitives); that it works consistently on all people; and that it convincingly produces lasting benefits. I am still waiting. I recognize that there has been an occasional person who had severe pain of the back or in some other location and experienced dramatic relief, or someone stopped smoking easily, etc. Such testimonies can be persuasive, but in no way add up to conclusive evidence.
When we choose to receive medical treatment from an acupuncturist, a serious concern is that of placing oneself in the hands of a person who has poor or no understanding as to proper diagnosis and treatment, thus allowing serious disease to continue without identification and proper care. Many diseases are difficult to recognize even by highly trained and experienced physicians.
Steven Barrett M.D. illustrates the above comment with this story:
A study published in 2001 illustrates the absurdity of TCM (traditional Chinese medicine) practices. A 40-year old woman with chronic back pain who visited 7 acupuncturists during a 2 week period was diagnosed with “Qi stagnation” by 6 of them, “blood stagnation” by 5, “kidney Qi deficiency” by 2, “yin deficiency” by 1, and “liver Qi deficiency” by 1. The proposed treatments varied even more. Among the 6 who recorded their recommendations, the practitioners planned to use between 7 and 26 needles inserted into 4 to 16 specific “acupuncture points” in the back, leg, hand, and foot. Of 28 acupuncture points elected, only 4 (14%) were prescribed by 2 or more acupuncturists. 28) Barrett, Stephen, M.D.; Quackwatch Home Page, Be Wary of Acupuncture, Qi Gong, and “Chinese Medicine,” p. 7 Jan. (2004).
One would think, that with the lack of studies reporting positive effects of acupuncture, interest in its use would subside; but just the opposite has happened. More young physicians who have embraced the Eastern philosophy have matured into experienced physicians and by their numbers alone have considerable influence. Many of them have been promoted to positions of leadership in medical institutions and schools. Public pressure to try these “wonderful methods” has caused many hospitals to offer some type of alternative therapies. A scientific investigational study on acupuncture and its potential for being physiologically therapeutic to certain disorders continue.
A physician is faced daily with common ailments that are difficult to treat, such as fibromyalgia, migraine headaches, and osteoarthritis of back, hips, knees, and fingers. The medications used in an attempt to control the ever present pain are of themselves fraught with problems and danger. So physician and patient alike are always looking for an effective and safe way to bring relief. The physical risks of using acupuncture are low and many feel that if it is not helpful, what have they lost? When pain is unrelenting, a person is driven to try anything suggested, and this is why “testimonials” as to the great benefit received by some type of therapy have ready followers. I will present three short summaries of studies, using acupuncture as therapy, done recently on fibromyalgia, migraine headaches, and osteoarthritis.
In the Annals of Internal medicine, July 2005, Dr. Dedra Buchwald of the University of Washington in Seattle, reported a study on fibromyalgia using acupuncture. Acupuncture was administered twice a week for twelve weeks. The final report was that people with fibromyalgia were no more likely to report decrease of pain than people who received acupuncture wherein needles were inserted into random locations rather than specific acupuncture points, or they received simulated acupuncture but without needles. 29) Reuters Health Information; (2005-07-05) Acupuncture may do little for fibromyalgia, http://www.reutershealth.com/archive/2005/07/05/elinelinks/2005070elin003.html
Reuters Health Information 2006-03-02, reported on a German study using acupuncture for migraine headaches. Nine hundred patients were randomly selected to receive Chinese traditional acupuncture, sham acupuncture, or drugs, all showed equal effectiveness. Drug therapy for migraine is far from satisfactory so this comparison does not reflect as much benefit for acupuncture as it may seem. 30) Reuters Health Information; 2006-03-02: Acupuncture shown to relieve migraines: study, http://www.reutershealth.com/archive/2006/03/02/eline/links/20060302eline006.html
The British medical journal, Lancet, July 9, 2005, carried an article by Dr. Claudia Witt, from Charite University Medical Centre in Berlin, in reference to a study she and her colleagues conducted on osteoarthritis. This study involved 294 patients, ages fifty to seventy-five years of age with osteoarthritis of the knee. The average pain intensity of the group was 40 (the higher the score the greater the pain). The final analysis reported 149 patients were assigned to acupuncture, 75 to minimal acupuncture (inserting needles in distant non-acupuncture points), and 70 to a waiting “control” group. The treatment groups received twelve treatments over eight weeks. At that point, average scores on a standard osteoarthritis scale were 26.9 point nine for the acupuncture group, 35.8 for the minimal acupuncture group and 49.6 for the controls. At 26 weeks and 52 weeks there were no differences between any group.
The editorialists, both from The Churchill in Oxford, UK conclude: ‘We are still some way short of having conclusive evidence that acupuncture is beneficial in arthritis or in any other condition, other than in a statistical or artificial way. 31) Reuters Health Information; (2005-07-08): acupuncture may ease knee arthritis, for a while, http://reutershealth.com/archive/2005/07/08 /eline/links/20050708eline019.html
Some might say, “but there was benefit for the migraine sufferer and drugs were not needed.” Allow me to speak of another factor not considered in any of these studies, that of the power of Satan. If a practitioner of acupuncture is a believer in the Eastern thought or Western occultism and the patient has allowed him or herself to participate in this technique that comes from Eastern mysticism, is it not possible that the power of Satan can cause apparent benefits? Are we not told in Rev. 13: 13, 14 that miracles will be manifest to deceive, and in Rev. 16:14 that these are spirits of devils?
Have there been studies showing a benefit from acupuncture? Yes, there have been. It seems that almost all of the studies I read have been on conditions that involve pain, nausea, or various types of discomfort. For these symptoms the studies will often show a positive benefit, however, those benefits are usually only mildly better than sham or no acupuncture. After a few weeks to three months the difference between those tested and the controls usually have returned to being equal.
Let us consider a study where acupuncture was used for control of nausea and vomiting caused by receiving chemotherapy, also a study of patients receiving radiation for cancer treatment of the throat and neck area and receiving acupressure therapy for the resulting xerostomia (dry mouth) reported in CA: A Cancer Journal for Clinicians volume 59/#9/September/October 2009. The studies used acupressure bands which caused pressure to be applied to a specific acupressure point on the wrist. Previous studies have shown acupressure bands to be beneficial for control of nausea. Peter Johnstone M.D. and William A. Mitchell Professor and chair of Radiation Oncology at the Indiana University School of Medicine report the study for chemotherapy nausea.
The study was divided so that there were controls not receiving therapy with acupressure bands as well as those wearing the bands. Rigid record taking was instituted of the time of nausea symptoms, the amount of medications taken to control nausea, and the number of times vomiting occurred for those receiving therapy as well as the control group.
At the conclusion of the study those receiving acupressure therapy had a reduction of nausea and associated symptoms of 28% and the controls a reduction of 5%. However when the records of how much anti-nausea medication was taken and the number of times vomiting occurred there was no difference between those taking the acupressure treatment and the controls.
Investigators at University of Texas M.D. Anderson Cancer Center in Houston tested acupressure on patients having received radiation to the neck area that resulted in xerostomia (dry mouth). They had patients record the degree of dry mouth and the amount of time it caused distress. They also tested the amount of increase of saliva in the mouth that occurred from the acupressure treatment.
The conclusion of the study was that there was very significant difference in relief of symptoms of those taking the acupressure treatment versus those not taking. However there was no difference in the amount of saliva produced between the two groups.
In the final evaluation of the two groups it was clear that those receiving acupressure therapy reported beneficial (subjective) results, yet the measurements in each of the two studies did not reveal a difference in physiological changes between therapy and no therapy (objective results). Dr. Johnstone states the following: “we have evidence now proving that a disconnect often exists between a patient’s reported symptoms and objective evidence of those symptoms.”
(emphasis added)
In June 2010 The Center for Inquiry Office of Public Policy located in Washington D.C. presented a paper entitled ACUPUNCTURE: A SCIENCE-BASED ASSESSMENT, a position paper from this center and authored by Robert Slack, Jr. This report brings an up to date assessment of the scientific status of acupuncture as revealed by improved testing techniques in the past several years. The optimistic conclusions about the effects reported by use of acupuncture in past research during the 1970-1990’s was due to the placebo effect, but was not recognized due to not having a placebo in testing. This new and changed understanding is a result of the development of “sham” acupuncture technique which has caused a “complete unraveling of nearly all acupuncture claims.” The 1997 National Institutes of Health report on acupuncture as being effective for nausea, headache, and dental pain now carries the following disclaimer.
This statement is more than five years old and is provided solely for historical purposes. Due to the cumulative nature of medical research, new knowledge has inevitably accumulated in this subject area(…) thus some of the material is likely to be out of date, and at worst simply wrong. 32) http://www.csicop.org/specialarticles/show/acupuncturrea_science-based_assessmentp.11
(emphasis added)
The Cochrane Collaboration, one of the world’s most trusted evaluator of medical literature, undertook a recent systematic review of the research concerning acupuncture. The results of this analysis were included in an article presenting recent acupuncture research by Edzard Ernst in The American Journal of Medicine. He states:
During the past ten years, however, researchers have begun to take a more rigorous look at acupuncture, designing studies that are properly randomized and adequately controlled for placebo effect. Though research is ongoing, an increasingly robust body of literature has accumulated showing that acupuncture has no intrinsic clinical value.
After discarding reviews that are based on only three or fewer primary studies, only 2 evidence-based indications emerge: nausea/vomiting and headache. Even this evidence has to be interpreted with caution; recent trials using […] placebos suggest that acupuncture has no specific effects in either of these conditions. (Ernst, 2008, 1027) 33) http://www.csicop.org/specialarticles/show/acupuncturre_a_science-based_assessmentp.2
In Acupuncture: A Science Based Assessment, Robert Slack, Jr. pointed out that there are many articles to be found that do conclude that there has been “encouraging effectiveness” from the use of acupuncture. For individuals that are not acquainted with scientific testing it seems that these types of articles present solid evidence of benefits of acupuncture. Truth in science is better demonstrated by studies that test by use of a double blind, randomly selected, and having 1) test group; 2) placebo group; 3) control group; and with a large number (hundreds) in each group. The evaluation of results will also be double blind, that is, the individual doing the acupuncture treatments will not be the person to do the evaluation. The person evaluating will not know which test group of individuals he is evaluating. This helps reduce bias and comes closer to revealing truth.
Slack further states that with the development of an effective sham—placebo technique of acupuncture testing, there has been much better evaluation, with the results indicating: 1) that real acupuncture is not more effective that when a placebo procedure is done; 2) for many conditions there is no benefit for either acupuncture or sham procedure.
In this same review by Robert Slack Jr. he mentions that there have been leading proponents of acupuncture and other alternative therapies, such as Andrew Weil M.D., that emphasize that these therapies have far less potential to cause harm than many conventional treatments. Therefore they should be judged by a “sliding scale” as to their value of effectiveness. The less the risk of side effects of therapy the less strict should be the criteria for effectiveness. This is not science; it is bias of the highest order. One cannot use two standards to evaluate therapeutic effectiveness decided upon the degree of potential side effects. It does, however, often enter into the decision as to whether to use a therapy or not. 34) Slack, Robert Jr., Acupuncture: A Science-Based Assessment, A Position Paper From the Center For Inquiry Office of Public Policy, June, (2010).
A study (638 patients) of the use of acupuncture and its effectiveness for chronic low back pain was reported in May 2009. This research study was conducted by Daniel Cherkin Ph.D. senior researcher with the Group Health Research Institute in Seattle Washington. Patients were divided into four groups:
1) standard acupuncture; 2) individualized acupuncture; 3) placebo acupuncture using tooth picks to touch the skin; 4) standard medical treatment without acupuncture.
The patients treated with any of the three styles of acupuncture were reported to fare better than no acupuncture. Dr. Cherkin concluded that acupuncture was beneficial in treatment of low back pain and that the study had stimulated the question as to how acupuncture works. Other scientists reviewing the study conclude that this study does not prove that acupuncture works, but that it shows the results are equal to use of a placebo; hence the obvious is that acupuncture of itself does not work. However, the lay press and proponents of acupuncture accept and voice the opinion that the study proved acupuncture is effective and does work. 35) Acupuncture for Chronic Low Back Pain, The New England Journal of Medicine, Boston, MA July 29, (2010); 363:454-61
The New England Journal of Medicine, July 29, 2010; 363:454-61 contained an article that reviewed recent research on acupuncture. In this scientific article the studies mentioned in the above paragraphs were included in its evaluation of acupuncture. This article in the NEJM originates from the Center for Integrative Medicine, University of Maryland School of Medicine and the University of Maryland Dental School; also from Department of Neurology and the Program in Integrative Health, University of Vermont College of Medicine, Burlington; and the Institute for Social Medicine, Epidemiology, and Health Economics, Charite’ University Medical Center, Berlin.
Integrative health programs seek to bring together therapies of Western scientific medicine and alternative (non science based therapies such as Ayurveda and traditional Chinese medicine) therapy. Thousands of offices and clinics across America and several medical schools have combined these methods. As seen by the names of the organizations behind this particular article one recognizes the potential bias to be expected, however I found the article to be quite scientific with an obvious attempt to avoid bias.
In this article a short explanation is presented of the Chinese theory of Ch’i and yin—yang, meridians, and Chinese traditional medicine’s concept of physiology that was presented earlier in this chapter. Then this statement is made on page 3:
…Efforts have been made to characterize the effects of acupuncture in terms of the established principles of medical physiology on which Western medicine is based. These efforts remain inconclusive, for several reasons…. 36) Ibid.,
These reasons are given in the following summary of findings from studies testing for physiologic changes from acupuncture performed mostly in animals;
- Acupuncture will activate peripheral-nerve fibers of all size.
- Acupuncture experience is dominated by a strong psychosocial context, including expectation, beliefs, and therapeutic milieu.
- Injecting the skin at the spot of presumed acupuncture point with a local anesthesia will block the analgesic effects of acupuncture.
- Endorphins are released by the brain-stem, sub-cortical and limbic parts of the brain.
- In rats electrical acupuncture has shown release of hydrocortisone from pituitary gland which, in turn, results in anti-inflammatory responses.
- MRI studies have revealed changes in the limbic and basal forebrain areas when prolonged acupunctures stimulation is done.
- Positron-emission tomography has shown that acupuncture increases u-opioid-binding for several days in the same brain areas as stated above.
- Acupuncture has mechanical stimulation effects on connective tissue.
- Adenosine is released at the site of needle stimulation.
- There is increase blood flow at the local site of acupuncture.
In spite of what may look like to some as powerful positive proof of the physiological action of acupuncture; the article in the New England Journal of Medicine, July, 29, 2010 states the following:
However, the various observations that have been made are not sufficient to permit a unified theory regarding the effect of acupuncture on mechanism of chronic pain. 37) Ibid.,.
The article tells us of a meta-analysis study (information of many studies placed into one study and analyzed) in 2008 which included 6359 patients with low back pain. The real acupuncture treatment was no more effective than sham treatment. However, with real or sham treatment there was subjective improvement over conventional treatment without acupuncture. This same finding was reported in the previously described Cochrane Collaboration Study. This information is to be found in the Supplementary Appendix available with the original article in the New England Journal of Medicine, July 29, 2010.
Two additional studies are referred to in this article in NEJM July 29, 2010, they come from German investigators. One study with 1162 patients over eight years compared real acupuncture versus sham procedure for chronic low back pain. There was little difference between the groups and at six months they were identical yet somewhat better than the control group that did not receive acupuncture. The other German study involved 3093 patients over seven years and this study on low back pain was measured by use of a questionnaire concerning reduced back function. Two groups were tested, one with conventional therapy and one with acupuncture. The acupuncture group had significant improvement above the non-acupuncture group as revealed by questionnaire. The results are taken from subjective responses of the patient.
Your attention is now directed to the setting in which acupuncture is delivered. In the traditional practice the insertion of the needle may be accompanied by a variety of other procedures, such as palpation of the radial artery in the wrist, as well as pulses in other locations. The tongue may be inspected in detail, recommendations as to use of herbs etc. All of these actions are based on the application of the principles of traditional Chinese medicine in contrast to Western scientific physiological medical concepts.
To the credit of the authors of this article we are not left at this point with the conclusion that acupuncture functions on a physiologic basis, actually they suggest its function may well be explained from a psychological standpoint and more research is needed in that direction. See quote below:
There is continuing debate in the medical community regarding the role of the placebo effect in acupuncture. As noted above, the most recent well powered clinical trials of acupuncture for chronic low back pain showed that sham acupuncture was as effective as real acupuncture. The simplest explanation of such findings is that the specific therapeutic effects of acupuncture, if present, are small, whereas it’s clinically relevant benefits are mostly attributable to contextual and psychosocial factors, such as patients’ beliefs and expectation, attention from the acupuncturist, and highly focused, spatially directed attention on the part of the patient. These studies also seem to indicate that needles do not need to stimulate the traditionally identified acupuncture points or actually penetrate the skin to produce the anticipated effect… 38) Dominique and Marie-Joseph Hoizey; A History of Chinese Medicine, UBC Press University of British Columbia, Vancouver, B.C, Canada (1993), pp.173–174.
In the closing part of this extensive article recommendation is given for additional studies to further evaluate the efficacy of sham (placebo) acupuncture without skin penetration, since it may be possible to achieve the same benefits by not doing invasive needle punctures. The master of Qi Gong tells us he can accomplish feats and healing equal to using needles in acupuncture simply by performing Qi Gong about a person. Light beams shined on the skin are said to work as well as needles, on and on it goes.
Wow, this reminds me of the experience of Mesmer, first he used magnets to effect healing, and then he learned he did not need magnets as he could accomplish the same simply by his hands. From there he moved on to the use of only the mind in bringing apparent healing; Mesmerism—hypnotism. In this chapter on traditional Chinese medicine I have not had the motive or desire to prove that the therapies are simply—fake. I believe at times quite remarkable changes may occur and apparent healing takes place, yet I ask the question BY WHAT OR WHOSE POWER DOES IT WORK? That is the concern.
For the past three thousand plus years the power of Eastern healing has been accepted and referred to a spiritual power. It is only in the last seventy-five to one hundred years has there been an attempt to describe its action in terms of modern physics. There is only one source of spiritual power, God Almighty the Creator of the universe and then God has allowed Satan a certain amount of power by which he can deceive.
Why do I warn against using therapies of traditional Chinese medicine if one does not believe in the astrological concepts upon which acupuncture is based, but only wants to take of the “good” of the method? I believe that as a person understands traditional Chinese medicine’s origin and theory of man being the microcosm of the macrocosm (universe) and that a balance of a two sided universal energy referred to as chi when rightly balanced created the universe and man and when out of balance creates illness and malfunction; it would be impossible to participate in these so called healing methods without acceptance of that power. Is it a treatment method that will cure infectious or chronic diseases or increased life span? Thus far no evidence has been presented to support such.
In China, for at least 3000 years, traditional Chinese medicine was part of medical care (acupuncture for 2000). What was the health status under this system? It was dismal. Neither public nor personal hygiene was practiced. Chairman Mao attacked these conditions head-on in the 1950’s and a national movement to improve hygiene personally and publicly was instituted. By the end of the 1950’s, great progress had been made in reducing infectious diseases. This was done by making changes that were scientific, not by practices based on astrological concepts of unbalanced energy. Clean water, closed sewer systems, cleanliness of body and homes, controlling vectors of infectious disease and parasites, and immunization brought improvement. [reference] Dominique and Marie-Joseph Hoizey; A History of Chinese Medicine, UBC Press University of British Columbia, Vancouver, B.C, Canada (1993), pp.173–174. [/reference] Life span doubled in fifty years; it was one of the most remarkable medical feats of the twentieth century.
As infectious diseases in China came under control and living habits along with diet changed to include use of more animal products, the degenerative diseases of the West began to replace infectious disease. Today, the # 1 cause of death in China is vascular disease, followed by cancer.
This has been a very brief glimpse of the most commonly used healing methods of traditional Chinese medicine, which have been practiced in China for at least 2000 or more years. The end result has been abysmal, and it took the introduction of scientific medicine to improve health and increase life span in China, doubling in fifty years. None of this can be attributed to traditional Chinese medicine.
What is so attractive about a system that has no proven track record of improving health? What causes us to flock to it as if it was something new and wonderful? Could it be we have accepted its spiritual philosophy and have chosen to partake of the “tree of knowledge of good and evil?”
In the next chapter, we will look at the emergence from the West of other energy balancing therapies.
References
| ↑1 | Lyons, Albert S., Petrucelli, R. Joseph II; Medicine An Illustrated History, Harry N. Abrams, Inc. Publishers, NY, (1978), p. 125. |
|---|---|
| ↑2, ↑3 | Ibid., p. 124. |
| ↑4 | McNamara, Sheila; Traditional Chinese Medicine, Basic Books, [Perseus Books] New York, NY, (1996), p. 26. |
| ↑5 | Kavoussi, Ben MS, MSOM, Lac, Science-Based Medicine, Astrology with Needles, pp.5,6; http://www.sciencebasedmedicine.org/?p=583 |
| ↑6 | McNamara, op. cit., p.117 |
| ↑7 | Ibid., p. 130. |
| ↑8 | Ibid., pp. 127–128. |
| ↑9, ↑10 | Ibid., p. 128. |
| ↑11 | Medical Tribune, Feb. 5, (1986) by Elizabeth Mechcatie (medical newspaper) |
| ↑12 | Ibid. |
| ↑13 | McNamara, op. cit., p. 128. |
| ↑14 | Ibid., p. 128. |
| ↑15 | U.S. News and World Report, Opiate of the Masses, by Bay Fang, Feb. 22, (1999), p. 45. |
| ↑16 | Basser, Stephen M.D.; Acupuncture: A History, Acupuncture Watch; http://www.acuwatch.org/hx/basser.shtm Feb. 22, (2005). |
| ↑17 | Epler, Jr DC., Bloodletting in early Chinese medicine and its relation to the origin of acupuncture. Basser, op.cit. p. 1 |
| ↑18 | Bassar, op. cit., p. 2. |
| ↑19 | Epler, Jr DC. Bloodletting in early Chinese medicine and its relation to the origin of acupuncture. Bull Hist Med. 1980l54L357-367; Reported in Basser, Ibid., p. 2 |
| ↑20 | Unschuld PU. Medicine in China: a History of Ideas, Berkeley, CA: University of California Press; (1985), Reported in Acupuncture Watch; Basser, op. cit., p. 2. |
| ↑21 | Unschuld PU. Nan-ching: The Classic of Difficult Issues. Berkeley, CA: University of California Press, (1986), p. 5; Reported in Basser, op. cit., p. 2. |
| ↑22 | Unschuld PU. Nan-ching op. cit., p. 5; Reported in Basser, op. cit., p. 2. |
| ↑23 | Ibid., p. 6. |
| ↑24 | Basser, op. cit., p. 8 |
| ↑25 | Sampson, Wallace I. M.D.; Acupuncture Watch, Critique of the NIH Consensus Conference on Acupuncture, March 2005, p. 2; http://www.acuwatch.org/general/nihcritique.shtml |
| ↑26 | Ibid., p. 2. |
| ↑27 | Linde K, Allais G, Brinkhaus B, Manheimer E, Vickers A, White AR. Acupuncture for tension-type headache. Cochrane Database of Systematic Reviews, Issue 1. Art. No.:CD007587 DOI: 10.1002/14651858.CDOO7587 Linde K, Allais G, Brinkhaus B, Manheimer E, Vickers A, White AR. Acupuncture for tension-type headache. Cochrane Database of Systematic Reviews, Issure 1. Ar. No.:CD001218 DOI. |
| ↑28 | Barrett, Stephen, M.D.; Quackwatch Home Page, Be Wary of Acupuncture, Qi Gong, and “Chinese Medicine,” p. 7 Jan. (2004). |
| ↑29 | Reuters Health Information; (2005-07-05) Acupuncture may do little for fibromyalgia, http://www.reutershealth.com/archive/2005/07/05/elinelinks/2005070elin003.html |
| ↑30 | Reuters Health Information; 2006-03-02: Acupuncture shown to relieve migraines: study, http://www.reutershealth.com/archive/2006/03/02/eline/links/20060302eline006.html |
| ↑31 | Reuters Health Information; (2005-07-08): acupuncture may ease knee arthritis, for a while, http://reutershealth.com/archive/2005/07/08 /eline/links/20050708eline019.html |
| ↑32 | http://www.csicop.org/specialarticles/show/acupuncturrea_science-based_assessmentp.11 |
| ↑33 | http://www.csicop.org/specialarticles/show/acupuncturre_a_science-based_assessmentp.2 |
| ↑34 | Slack, Robert Jr., Acupuncture: A Science-Based Assessment, A Position Paper From the Center For Inquiry Office of Public Policy, June, (2010). |
| ↑35 | Acupuncture for Chronic Low Back Pain, The New England Journal of Medicine, Boston, MA July 29, (2010); 363:454-61 |
| ↑36 | Ibid., |
| ↑37 | Ibid.,. |
| ↑38 | Dominique and Marie-Joseph Hoizey; A History of Chinese Medicine, UBC Press University of British Columbia, Vancouver, B.C, Canada (1993), pp.173–174. |
